An HVAC system in pharma is the engineered set of air-handling equipment and controls that maintains the required cleanliness, temperature, humidity, airflow direction, and pressure cascade in manufacturing and support areas—so products are protected from contamination and cross-contamination, and (where needed) hazardous materials are contained. World Health Organization
What pharma HVAC must achieve
- Air cleanliness control: limits airborne particles and (in cleanrooms) supports microbial control through appropriate filtration and room design.
- Pressure differentials (pressure cascade): air should generally flow from cleaner to less clean areas (or the reverse for containment of potent/toxic materials). For sterile areas, EU GMP Annex 1 gives a guidance value of ≥ 10 Pa pressure difference between adjacent rooms of different grades.
- Continuous monitoring & alarms: for critical differentials, pressure should be continuously monitored/recorded with warning systems for failures or drops below set limits.
- Comfort and process control: temperature and RH must not adversely affect product quality or equipment performance. World Health Organization
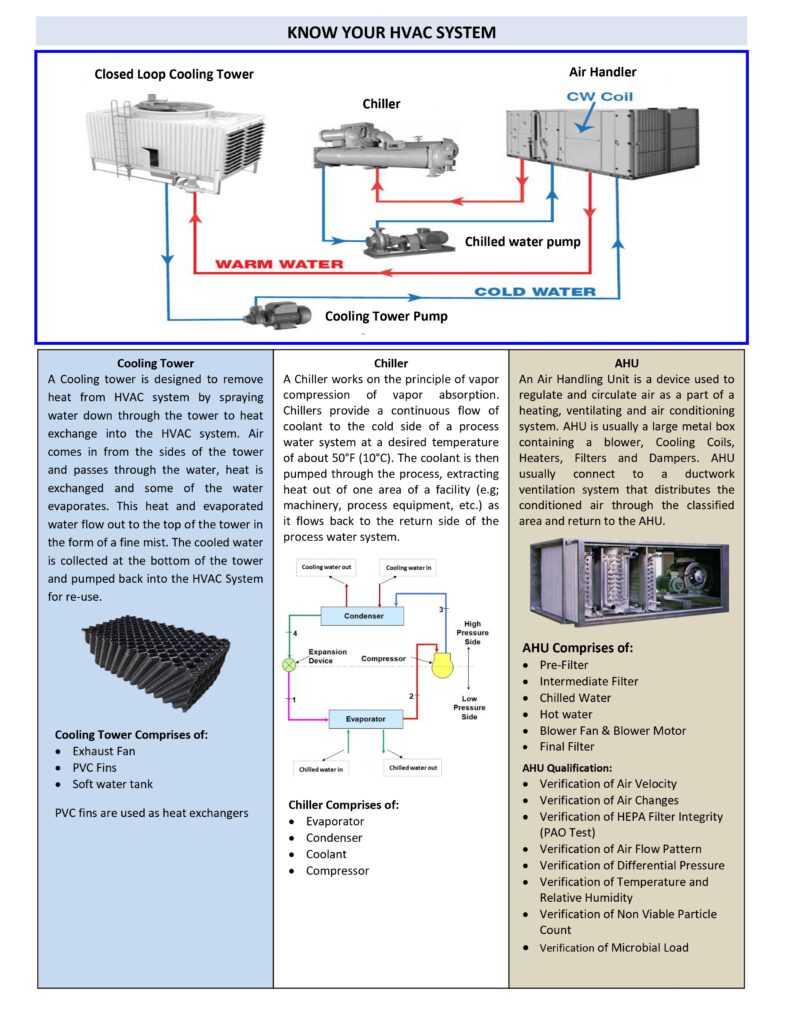
Main components
- Air Handling Unit (AHU): mixes/conditions air; includes cooling/heating coils, humidification/dehumidification, and pre/medium filters.
- Final (terminal) filtration: often HEPA filters at room terminals for controlled areas.
- Supply/return/exhaust ducting: delivers air to critical zones and removes air from low points/dust sources as required.
- Room terminals: diffusers (including unidirectional airflow terminals for aseptic critical zones), return grilles, pressure relief dampers.
- Controls & instrumentation: DP transmitters, temperature/RH sensors, airflow/velocity controls, BMS/SCADA trending and alarms.
Cleanroom standards and classification
Cleanrooms are classified using particle concentration criteria (commonly aligned with ISO cleanroom concepts). ISO 14644-1 specifically defines classification of air cleanliness by airborne particle concentration. ISO
Qualification and routine checks
Typical HVAC qualification/verification includes:
- HEPA integrity testing, airflow volume/velocity and air change verification
- Pressure differential mapping, alarm challenge tests
- Airflow visualization (smoke studies) to confirm airflow direction and no ingress to higher grade zones
- Temperature/RH mapping and ongoing monitoring/trending
If you tell me your area (tablet / sterile / ointment), I can list the typical HVAC setpoints and monitoring points used for that area.
tablet / sterile / ointment
Thought for 57s
Here are typical HVAC setpoints and monitoring points for tablet / sterile / ointment areas (final values must be justified by your CCS/QRM, product needs, and facility design).
Tablet area (OSD manufacturing)
Typical setpoints
- Temperature: ~20–25 °C (set for operator comfort + process stability).
- RH: commonly 40–60% RH; for moisture-sensitive steps (sieving, compression, some actives) you may need lower RH with tighter control.
- Pressure cascade: chosen to prevent cross-contamination; for containment, ~15 Pa is often used and 5–20 Pa may be acceptable depending on design and tolerance.
- Use local dust extraction; HVAC should not be the primary dust control method.
Key monitoring points
- Room DP (between rooms/airlocks; with alerts/action limits).
- Temp/RH (monitored + recorded where relevant).
- Dust extraction performance (airflow, duct build-up checks)
- Filter ΔP (pre/HEPA where used), supply/return airflow balance, air changes (as per qualification).
Sterile area (aseptic / cleanrooms)
Typical setpoints (critical)
- Pressure differential: ≥10 Pa between adjacent rooms of different grades (guidance).
- Unidirectional airflow (Grade A zones): 0.36–0.54 m/s at working position (guidance), justified in qualification/CCS.
- Temp/RH: controlled/recorded as needed for product and personnel comfort (values are site-defined).
Key monitoring points
- Continuous particle monitoring in Grade A during critical processing, with ≥28.3 L/min (1 ft³/min) sample flow and alarms on alert/action exceedance.
- Viable monitoring (air/surface/personnel) frequency based on risk and CCS.
- DP cascade continuous trending; HEPA integrity, airflow volume/velocity, airflow visualization (smoke), recovery—part of qualification and periodic checks.
Ointment area (non-sterile creams/ointments; and sterile ophthalmic where applicable)
Typical setpoints
- Non-sterile ointment: temperature/RH controlled to protect product and reduce microbial risk (site-defined ranges).
- Pressure cascade: set based on product protection vs containment (e.g., dusty powders, potent actives); 15 Pa often used, 5–20 Pa may be acceptable.
- Sterile ophthalmic ointment: follow sterile cleanroom expectations (DP, Grade A airflow, monitoring).