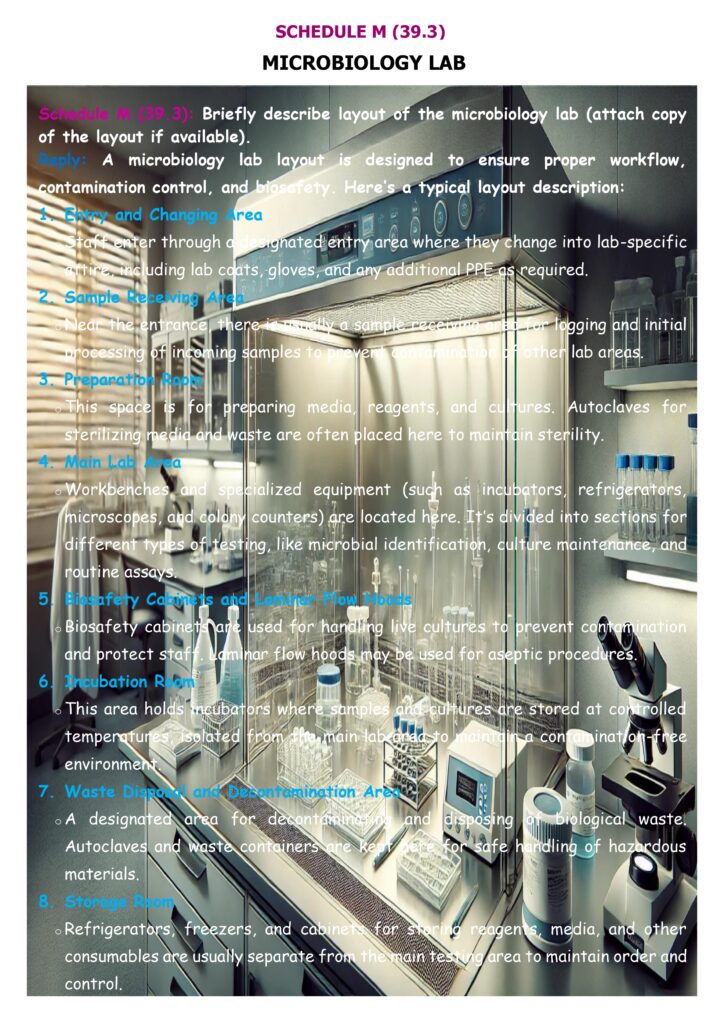
Schedule M – Point 39.3 (Microbiology Lab) in a Risk-Based Inspection (RBI) focuses on whether the firm has an appropriate microbiology laboratory layout and can briefly describe it (with a layout drawing, if available). CDSCO In RBI, this point is treated as high-impact because poor layout can cause false positives/false negatives, cross-contamination of cultures, and unreliable microbiological decisions affecting batch release.
What “layout” should demonstrate (what inspectors expect)
Inspectors typically expect the layout description/drawing to clearly show:
- Dedicated, separated microbiology lab and support equipment (e.g., autoclaves, glassware handling) away from production areas.
- Sufficient space and defined zones for samples, reference organisms, media (including cold storage if needed), testing benches, incubators, and records—so activities don’t overlap and create mix-ups.
- Segregation of activities (by space or by time): sample preparation, media/equipment prep, and enumeration/handling of cultures should not interfere with each other; sterility testing must be in a dedicated area.
- Separate air supply / separate AHU provisions for microbiology labs, with suitable temperature/humidity control and air quality that does not become a contamination source.
- Restricted access and defined entry/exit & gowning rules, aligned to containment needs.
For facilities performing sterility testing, RBI often goes deeper: WHO expects sterility testing under aseptic conditions equivalent to sterile manufacturing standards, typically Grade A unidirectional airflow (or equivalent) within a Grade B background, and the layout should prevent disruption of airflow patterns.
How RBI verifies compliance (practical checks)
RBI inspectors usually:
- Compare the layout drawing with the actual lab walk-through (flows of people, samples, waste, cultures).
- Check whether zoning supports prevention of cross-contamination and reduces risk of erroneous results (false positives/negatives).
- Sample evidence that high-risk zones are controlled (access logs, EM where applicable, cleaning/disinfection, incident handling).
- Escalate inspection depth when microbiology risk is high, consistent with risk-based inspection planning principles (scope and intensity adjusted to patient/product risk).
Common RBI gaps: no dedicated sterility area, crowded/overlapping zones, shared storage for sterile media and cultures, poor airflow segregation, and layouts that don’t match real operations.