
Fogging in pharma is a whole-room disinfection method where a disinfectant is aerosolized into a fine mist (fog) to cover all exposed surfaces and the air in controlled areas like cleanrooms and sterile production zones. It is an additional step, not a replacement for manual cleaning and routine disinfection.
Below is a practical, pharma-focused detailed write-up you can almost use as a ready article/SOP backbone.
1. What Is Fogging in Pharma?
Fogging (often called fumigation or whole-room bio-decontamination) is the process of dispersing a disinfectant as very fine droplets into a cleanroom or controlled environment so that:
- The air and hard-to-reach surfaces (behind equipment, ceiling, duct grills, etc.) are exposed to the disinfectant.
- A validated contact time is achieved to reduce microbial load to a predefined level (often aiming for ≥ 4–6 log reduction for key challenge organisms, depending on risk & agent). blog.pegasusclean.com+1
In pharma, fogging is typically used for:
- Sterile manufacturing areas (Grades A/B background, C, D – as per CCS and local procedures).
- Microbiology labs, isolators and biosafety cabinets. Curis System+1
- Recovery after construction/maintenance work, contamination excursions, or major shutdown.
2. Common Types of Fogging Systems
- Cold Fogging / ULV (Ultra Low Volume) Fogging
- Uses mechanical nozzles/rotary discs to generate fine droplets (typically 5–50 µm).
- Suitable for many pharma cleanrooms and support areas. cleanroomtechnology.com+1
- Thermal Fogging
- Uses heat to vaporize solution into visible fog.
- Less common in regulated pharma cleanrooms due to material compatibility, heat, and safety concerns.
- Vaporized / Ionized Hydrogen Peroxide (VHP / iHP) – often termed fumigation
- Hydrogen peroxide (often 7–35%) is vaporized or ionized and actively distributed.
- Offers reproducible, high-level decontamination; commonly validated with Geobacillus stearothermophilus biological indicators (BIs). Pharmaguideline+1
3. Disinfectants Used for Fogging
Typical choices (must be justified in the Contamination Control Strategy – CCS):
- Hydrogen Peroxide (H₂O₂)
- Broad-spectrum (bacteria, viruses, fungi, spores).
- Breaks down into water and oxygen, leaving minimal residue. blog.pegasusclean.com+2tecomak.com+2
- Used as mist, vapor, or ionized fog.
- Hydrogen Peroxide + Silver / Other Synergists
- Combination products (e.g., ~11% H₂O₂ + silver nitrate) marketed for surface and fogging disinfection in hospitals and cleanrooms. vodachemicals.com
- Peracetic Acid (PAA)-Based Systems (often as dry fog)
- Highly sporicidal; used in biosafety cabinets and some cleanrooms. PMC
- (Legacy) Formaldehyde Fogging – Now Largely Obsolete/Banned
- Historically used but now discouraged/banned due to carcinogenicity and worker safety issues; most sites have switched to H₂O₂/VHP or other safer systems. Pharmaguideline+1
Regulatory note: EU GMP Annex 1 (2022) does not mandate fogging but expects a robust, risk-based cleaning & disinfection program, including validated methods and use of sporicidal agents where appropriate. Pharma Now
4. When Is Fogging Used?
Fogging is typically applied:
- After major maintenance, construction, or shutdown in Grade B/C/D areas.
- Following environmental monitoring excursions (trend-based or out-of-limit results) as part of corrective action. pharmadevils.com+1
- Before starting aseptic operations after prolonged idle periods.
- Periodically, if justified in CCS, for high-risk areas (e.g., isolators, lyophilizer chambers, certain high-risk Grade C/D).
It is not generally used as a routine, daily disinfection step; regulators (e.g., CDC) caution against routine fogging in healthcare areas due to limited added benefit versus risk, unless justified. CDC
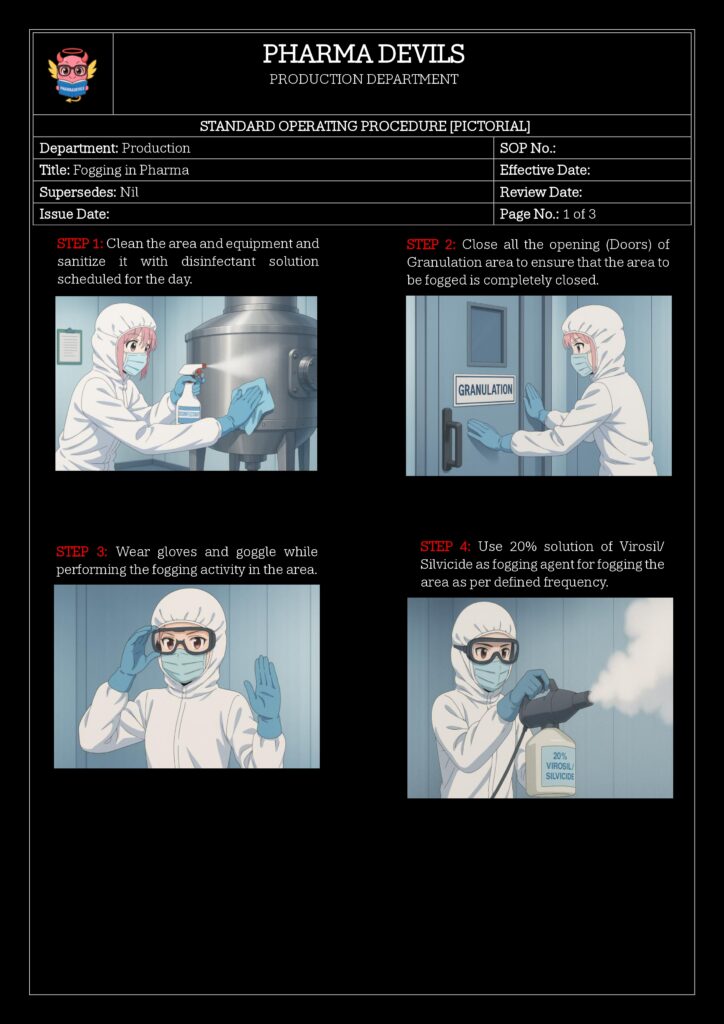
5. Pre-Fogging Requirements (Prerequisites)
Before fogging:
- Perform Manual Cleaning First
- Remove gross soil, dust, and residue with approved detergent/disinfectant.
- Fogging is not effective on heavy organic load. Pharma Now+1
- Verify Area Status
- Ensure the area is vacant (no personnel).
- Stop ongoing operations, cover/remove open product and direct contact components.
- Protect Sensitive Equipment
- Cover or remove sensitive electronics, paper records, and corrosion-prone items if not qualified to withstand the agent.
- Seal the Area as per Procedure
- Close doors, windows, pass boxes, dampers as required to maintain fog concentration. Pharmaceutical Microbiology Insights+1
- HVAC Settings
- Either keep AHU running on a defined cycle (to assist distribution) or switch to a predefined mode (e.g., minimum exhaust) as justified in validation.
6. Typical Fogging Procedure – Step-by-Step
This is a generic outline. Site SOP must be based on actual equipment, agent, and validation data.
- Planning & Authorization
- Initiate fogging via approved request (BMR/BPR reference, deviation CAPA, or planned preventive activity).
- Verify that the correct disinfectant, batch number, and expiry are available.
- Calculate Disinfectant Quantity & Cycle Time
- Volume of room (m³) × validated dose (e.g., ml/m³ or g/m³) → required quantity.
- Cycle duration should include dispersion time + minimum contact time (commonly 15–30 min or as per validation for the specific system). cleanroomtechnology.com+1
- Place Fogger(s)
- Central location or as per layout mapping to ensure uniform coverage (multiple units for large/complex rooms). Pharmaceutical Microbiology Insights+1
- Place Indicators (for Validation / Routine Check)
- Biological indicators (BIs) and/or chemical indicators (CIs) at worst-case locations:
- Corners, behind equipment, under benches, on high shelves, inside isolator chamber, etc.
- Common BI: Geobacillus stearothermophilus spore coupons for H₂O₂/VHP systems. Pharmaguideline+1
- Biological indicators (BIs) and/or chemical indicators (CIs) at worst-case locations:
- Start Fogging Cycle
- Start the fogger and exit the area, ensuring doors are properly closed.
- Observe status via external indicator or HMI if provided.
- Hold / Contact Time
- Maintain area sealed for validated contact time (e.g., 30–90 min, or as per system).
- HVAC mode should be the same as used during validation (e.g., reduced exhaust, recirculation, or off). cleanroomtechnology.com+1
- Aeration / Ventilation
- After contact time, start controlled aeration:
- Open specific vents/doors or use AHU to bring concentration down below occupational exposure limits.
- Many modern systems monitor H₂O₂ concentration and signal when safe levels are reached. Curis System+1
- After contact time, start controlled aeration:
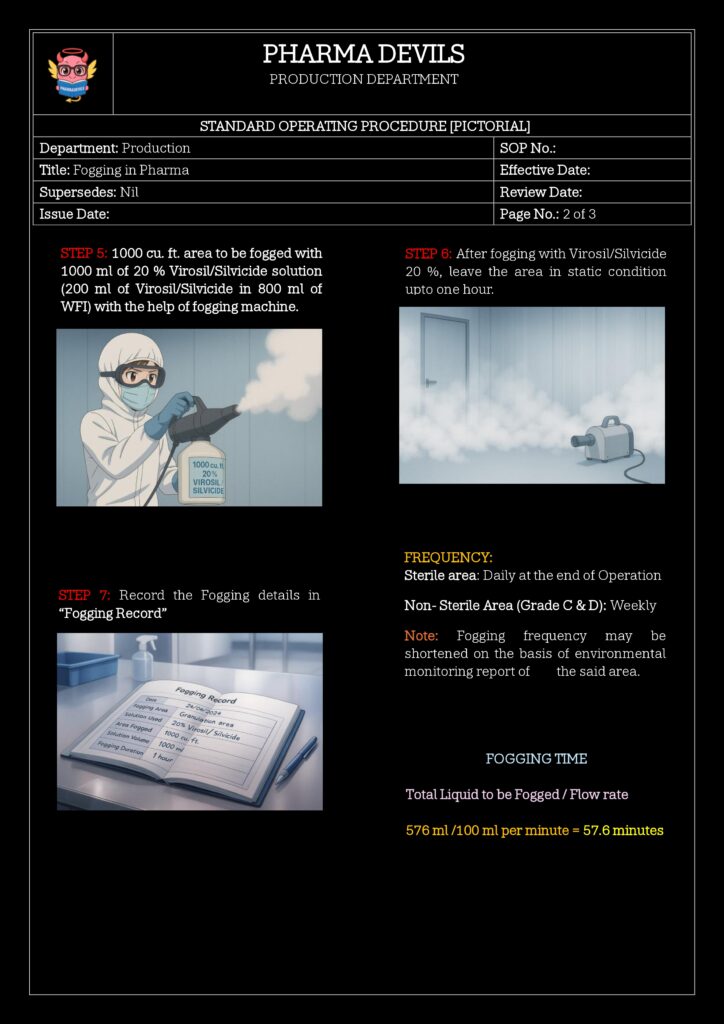
- Post-Fogging Checks & Documentation
- Retrieve BIs/CIs and send to microbiology for incubation (BIs) or visual reading (CIs).
- Record:
- Date, time, area, disinfectant details, quantity, room volume, operator, results of BIs/CIs, deviations, and clearance to use area.
7. Validation and Re-Qualification of Fogging
Fogging must be fully validated as part of the disinfection program:
7.1 Initial Validation
- Worst-Case Study Design
- Choose largest room volume, maximum load/obstructions, lowest temperature/humidity within operating range.
- Place multiple BIs and CIs throughout, focusing on shielded and hard-to-reach spots. Pharmaguideline+2PMC+2
- Number of Runs
- Typically at least three consecutive successful cycles to demonstrate reproducibility.
- Acceptance Criteria
- BIs: No growth (or defined log reduction) after incubation.
- CIs: Required color change indicating adequate exposure.
- Environmental / surface monitoring post-fogging supports overall microbial reduction.
- Safety & Material Compatibility
- Confirm no unacceptable damage/corrosion to room finishes, HEPA filters, instruments and stainless steel.
7.2 Ongoing Re-Qualification
- At defined intervals (e.g., annually) or upon:
- Major change in room layout, volume, or surfaces.
- Change in disinfectant product, concentration, or fogging system.
- Significant deviation or failure trend (recurring high counts). Pharma Now+1
8. Advantages of Fogging in Pharma
- Improved Coverage:
- Reaches inaccessible surfaces such as ducts, cable trays, undersides of equipment, and complex geometries. cleanroomtechnology.com+1
- High-Level Decontamination:
- VHP/iHP systems can achieve very high log reductions and are suitable for high-risk operations. Curis System+1
- Reduced Manual Burden:
- Complements manual disinfection; useful for large volumes where wiping alone is impractical.
9. Limitations and Risks
- Not a Substitute for Cleaning
- Organic load and visible dirt must be removed first, otherwise efficacy drops sharply. Pharma Now+1
- Worker Safety & Regulatory Concerns
- Incorrect agents or poorly controlled fogging can expose staff to irritants/toxins.
- Healthcare regulators like CDC do not recommend routine environmental fogging in patient-care areas because of safety and limited proven benefit when standard cleaning is adequate. CDC
- Residues & Material Compatibility
- Some agents can leave residues or cause corrosion if not properly selected and validated.
- Cycle Time & Downtime
- Area must be empty, sealed, fogged, and then aerated → not suitable for very frequent use unless system is highly optimized.